Basal Cell Carcinoma
What is basal cell carcinoma?
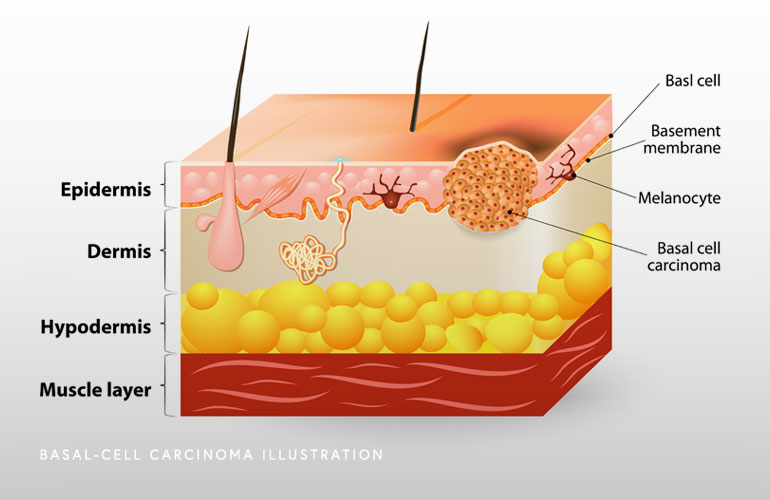
Basal cell carcinoma (BCC) is the most common form of skin cancer. Over three million cases are diagnosed annually in the United States. Basal cells are stem-cells that produce new skin cells when old ones mature. Most basal cell carcinoma are slow growing. While basal cell carcinoma rarely metastasizes or spreads to other parts of the body, it can grow locally, invading and destroying surrounding tissues including muscle, bone and cartilage if left untreated. Sun exposure, particularly to ultraviolet (UV) rays, is the primary risk factor for developing basal cell carcinoma. Early detection and treatment are crucial for effectively managing basal cell carcinoma and preventing cancer progression.
If you or a loved one has been diagnosed with basal cell carcinoma, the most common type of skin cancer, consult a board-certified dermatologist at Apex Skin Center. Our skilled team, regarded as top dermatologists in Cary, Apex, Holly Springs, and Fuquay-Varina, is committed to providing effective, compassionate treatment options tailored to your needs. With offices across the region, we make it easy to access the best in skin cancer care. Schedule an appointment today to learn more about your treatment options for basal cell carcinoma.
At a Glance
Dr. Thomas Knackstedt
- Double board certified in dermatology and Mohs Surgery
- Over ten years of experience providing evidence-based care
- Nationally renowned physician leader with numerous publications, lectures, and academic affiliations
- Learn more
