Acne
What is acne?
Acne is the most common skin condition in the United States, affecting up to 50 million Americans annually. Acne commonly begins during adolescence, affecting approximately 85% of teenagers between the ages of 12 and 24. However, it can persist into adulthood and even develop for the first time in individuals well into their 30s, 40s, and beyond. Acne can range from mild to severe and may cause discomfort, pain, and self-esteem issues for affected individuals, no matter what age. The face, back, and chest may be affected. Effective management of acne often requires a tailored approach. Consulting with a dermatologist can help determine the most appropriate treatment plan for addressing acne and minimizing its impact on overall skin health and well-being.
Acne can manifest in various forms, and its symptoms may vary depending on the severity and type of acne. Common symptoms include:
- Comedones: Comedones, or blackheads and whiteheads, are non-inflammatory acne lesions. Blackheads occur when pores become clogged with oil and dead skin cells, causing them to open and appear black on the surface of the skin. Whiteheads, on the other hand, occur when the pores are clogged but remain closed, resulting in small, flesh-colored bumps.
- Papules: Papules are small, raised, red bumps on the skin caused by inflammation and bacterial infection of the hair follicles. They may be tender to the touch and can occur individually or in clusters.
- Pustules: Pustules are similar to papules but contain pus, giving them a white or yellowish appearance at the center. They are often filled with inflammatory cells and bacteria and may be surrounded by redness and swelling.
- Nodules: Nodules are large, solid, painful lumps beneath the surface of the skin. They develop when clogged pores and inflammation extend deep into the skin, causing tissue damage and scarring. Nodular acne can be severe and may require medical intervention to prevent scarring and complications.
- Cysts: Cysts are deep, pus-filled lesions that are larger and more severe than pustules. They are often painful and can cause significant inflammation and tissue damage. Cystic acne is a severe form of acne that can lead to scarring and permanent skin damage if left untreated.
- Scarring: In severe cases of acne, scarring may occur as a result of tissue damage and inflammation. Acne scars can be shallow or deep, and they may appear as pitted or raised areas on the skin. Scarring can have a significant impact on an individual’s self-esteem and quality of life.
These symptoms can vary in severity and may cause discomfort, pain, or psychological distress for affected individuals. Seeking prompt treatment from a board-certified dermatologist can help manage symptoms, prevent complications, and improve overall skin health and appearance.
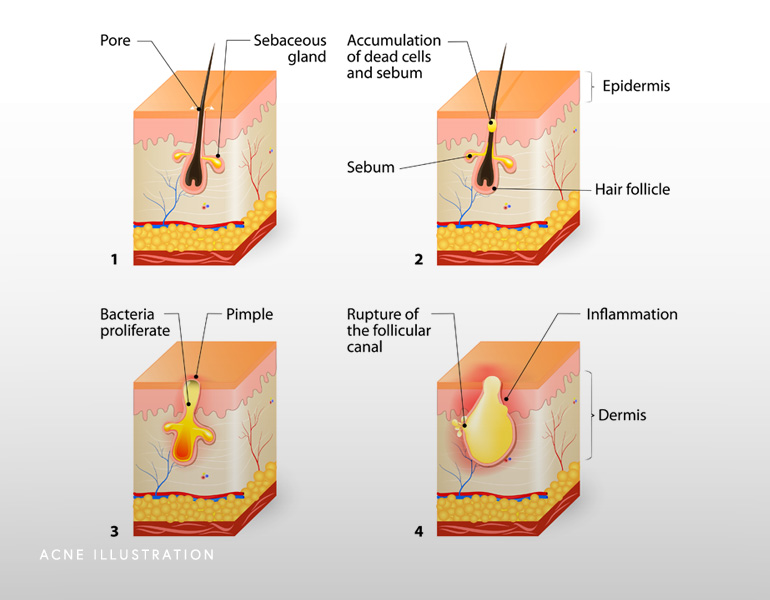
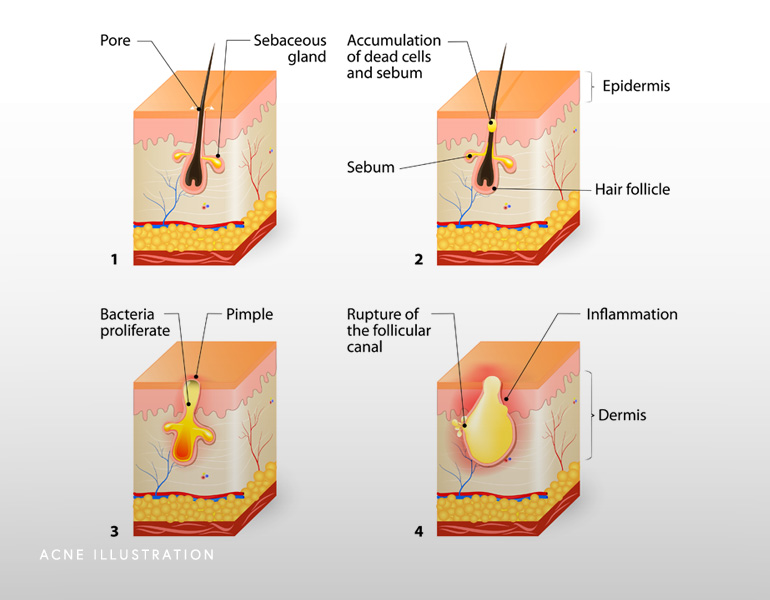
Acne occurs when hair follicles become clogged with oil and dead skin cells, leading to the formation of comedones (blackheads and whiteheads), as well as inflammatory lesions such as papules, pustules, nodules, and cysts. Several factors contribute to the development of acne:
- Excess Oil Production: The sebaceous glands in the skin produce an oily substance called sebum, which helps lubricate and protect the skin. However, excess sebum production, often influenced by hormonal changes, can lead to the clogging of hair follicles and the formation of acne lesions.
- Hormonal Changes: Hormonal fluctuations, particularly during puberty, menstruation, pregnancy, and menopause, can stimulate the sebaceous glands to produce more sebum. Androgens, a group of hormones including testosterone, play a significant role in regulating sebum production and are often elevated during puberty.
- Bacteria: Propionibacterium acnes (P. acnes), a type of bacteria that naturally resides on the skin, can proliferate in clogged pores and contribute to inflammation and the development of inflammatory acne lesions. These bacteria produce substances that trigger an immune response, leading to redness, swelling, and pus formation.
- Inflammation: Inflammatory mediators released by the immune system in response to bacterial colonization and other factors contribute to the inflammation seen in acne lesions. Inflammation plays a central role in the formation and progression of acne and can exacerbate existing lesions.
- Genetics: Acne often runs in families, suggesting a genetic predisposition to the condition. Individuals with a family history of acne may be more prone to developing the condition themselves due to inherited factors influencing sebum production, inflammation, and skin cell turnover.
- Dietary Factors: While the role of diet in acne is still under investigation, certain dietary factors, such as high glycemic index foods (e.g., sugary and processed foods) and dairy products, may exacerbate acne in some individuals. These foods can influence hormone levels and inflammation, potentially contributing to acne development.
- Stress: Psychological stress can trigger hormonal changes and exacerbate inflammation, potentially worsening acne symptoms. While stress alone is unlikely to cause acne, it may aggravate existing acne or contribute to flare-ups.
Medical History
The team at Apex Skin Center will begin by asking about your medical history, including any symptoms you are experiencing, the duration and pattern of those symptoms, previous skin conditions or treatments, family history, and any potential triggers or exacerbating factors.
Physical Examination
Board-certified dermatologist Dr. Knackstedt will conduct a thorough examination of the skin, looking for characteristic signs of acne.
Skin Biopsy (if necessary)
In some cases, a skin biopsy may be performed to confirm the diagnosis of acne and rule out other skin conditions with similar features. During a skin biopsy, a small sample of skin tissue is removed and examined under a microscope by a pathologist to look for characteristic histopathological changes consistent with acne. In most cases of acne, this is not necessary.
Acne treatment aims to reduce oil production, prevent clogging of pores, eliminate bacteria, and reduce inflammation to clear existing lesions and prevent new ones from forming. Treatment approaches may vary depending on the severity and type of acne, as well as individual factors such as skin type and medical history. Common acne treatments include:
- Topical Treatments: Over-the-counter and prescription topical treatments containing ingredients such as salicylic acid, retinoids (such as tretinoin, adapalene, and tazarotene), and antibiotics (such as clindamycin and erythromycin) can help unclog pores, reduce inflammation, and kill acne-causing bacteria.
- Oral Medications: Oral medications may be prescribed for moderate to severe acne or acne that is resistant to topical treatments. These may include oral antibiotics (such as doxycycline, minocycline, or tetracycline) to reduce inflammation and kill bacteria, oral contraceptives (for females) to regulate hormones and reduce sebum production, and oral isotretinoin (commonly known as Accutane) for severe, cystic acne that does not respond to other treatments.
Procedures: In addition to medications, certain procedures performed by dermatologists can help improve acne symptoms. These may include:
- Extraction: Manual extraction of comedones (blackheads and whiteheads) can help unclog pores and improve the appearance of the skin.
- Chemical Peels: Chemical peels use exfoliating agents to remove dead skin cells and unclog pores, resulting in smoother, clearer skin.
- Corticosteroid Injections: Intralesional corticosteroid injections can quickly reduce inflammation and shrink large, painful acne lesions such as cysts and nodules.
Skincare Routine: Adopting a gentle skincare routine tailored to acne-prone skin can help manage symptoms and prevent flare-ups. This may include using non-comedogenic (non-pore-clogging) cleansers, moisturizers, and sunscreen, avoiding harsh or abrasive products, and avoiding picking or squeezing acne lesions, which can worsen inflammation and lead to scarring.
Treatment for acne is often individualized based on the severity and type of acne, as well as the individual’s skin type, medical history, and treatment goals. It may take time to find the most effective treatment regimen, and consistent use of medications and skincare products is essential for achieving and maintaining clear skin. Consulting with a board-certified dermatologist can help determine the most appropriate treatment plan for managing acne and improving overall skin health and appearance.
If you or a loved one is struggling with acne, schedule a consultation with a board-certified dermatologist at Apex Skin Center. Our medical dermatology team in Cary, Apex, Holly Springs, and Fuquay-Varina specializes in treating acne with personalized solutions tailored to your skin type and condition. With advanced treatments and a compassionate approach, we’re committed to helping you achieve clear, healthy skin. Visit one of our convenient locations to start your journey toward effective acne management today.
At a Glance
Dr. Thomas Knackstedt
- Double board certified in dermatology and Mohs Surgery
- Over ten years of experience providing evidence-based care
- Nationally renowned physician leader with numerous publications, lectures, and academic affiliations
- Learn more