Melanoma
What is melanoma?
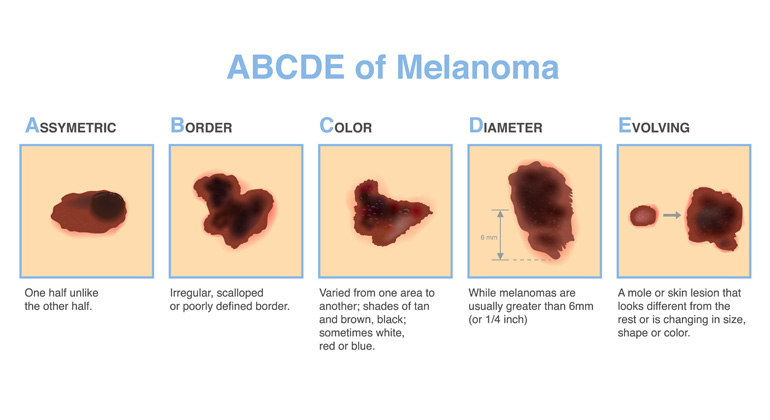
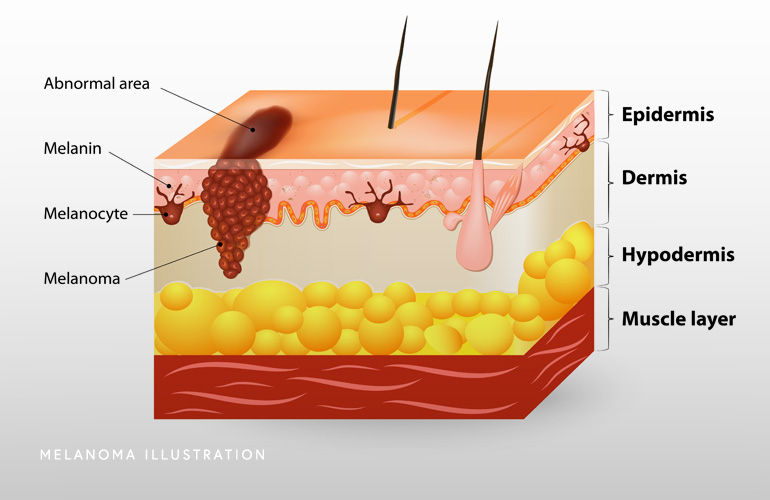
Melanoma is the third most common form of skin cancer and is far less common than basal cell carcinoma and squamous cell carcinoma. Approximately 100,000 cases are diagnosed annually in the United States. North Carolina ranks 17th in new cases of melanoma. Melanoma is the cancer that develops from melanocytes, the specialized pigment-producing cells in the skin. Most melanoma are diagnosed at an early stage when they are still highly treatable and curable. However, melanoma can be potentially serious. While melanoma accounts for only about 1% of all skin cancers, it causes the majority of skin cancer-related deaths. The depth or thickness (called Breslow’ thickness) of the melanoma primarily determines the probability that a melanoma spreads to the lymph nodes or other organs. Sun exposure, particularly to ultraviolet (UV) rays, is the primary risk factor but melanoma can also arise in skin not frequently exposed to the sun. Early detection and treatment are crucial for effectively managing melanoma and preventing cancer progression.
If you or a loved one is facing a melanoma diagnosis, schedule a consultation with a board-certified dermatologist at Apex Skin Center. Known throughout Cary, Apex, Holly Springs, and Fuquay-Varina as leaders in skin cancer care, our dermatologists offer expert, individualized treatment plans for melanoma. We are here to support you with advanced diagnostics and comprehensive treatment options at any of our convenient locations. Take the next step in managing melanoma with a trusted team by your side. Schedule your appointment today.
At a Glance
Dr. Thomas Knackstedt
- Double board certified in dermatology and Mohs Surgery
- Over ten years of experience providing evidence-based care
- Nationally renowned physician leader with numerous publications, lectures, and academic affiliations
- Learn more